Understanding the Differences in Prolapse - Anatomical vs. Symptomatic
Hey there, amazing mamas! Today, we're diving into a topic that's a bit like the hidden side of the moon – prolapse. And no, we're not talking about telescopes and astronauts here, but rather the nitty-gritty of your pelvic health. As a pelvic floor physical therapist, you're likely well aware of the ins and outs, but let's break it down for all you incredible moms out there.
What's Prolapse Anyway?
Okay, before we jump into the distinctions, let's get the basics down. Prolapse is when your pelvic organs decide they want to take a little vacation from their usual positions. Imagine your uterus, bladder, or rectum deciding to pack their bags and camp out in places they shouldn't be – like a family road trip gone wrong.
Anatomical Prolapse: The Where & How
So, let's start with the first star of our show: anatomical prolapse. This one's all about the "where." In anatomical prolapse, it's all about the position of your pelvic organs – whether they're making an unscheduled stop downward.
Here's the breakdown:
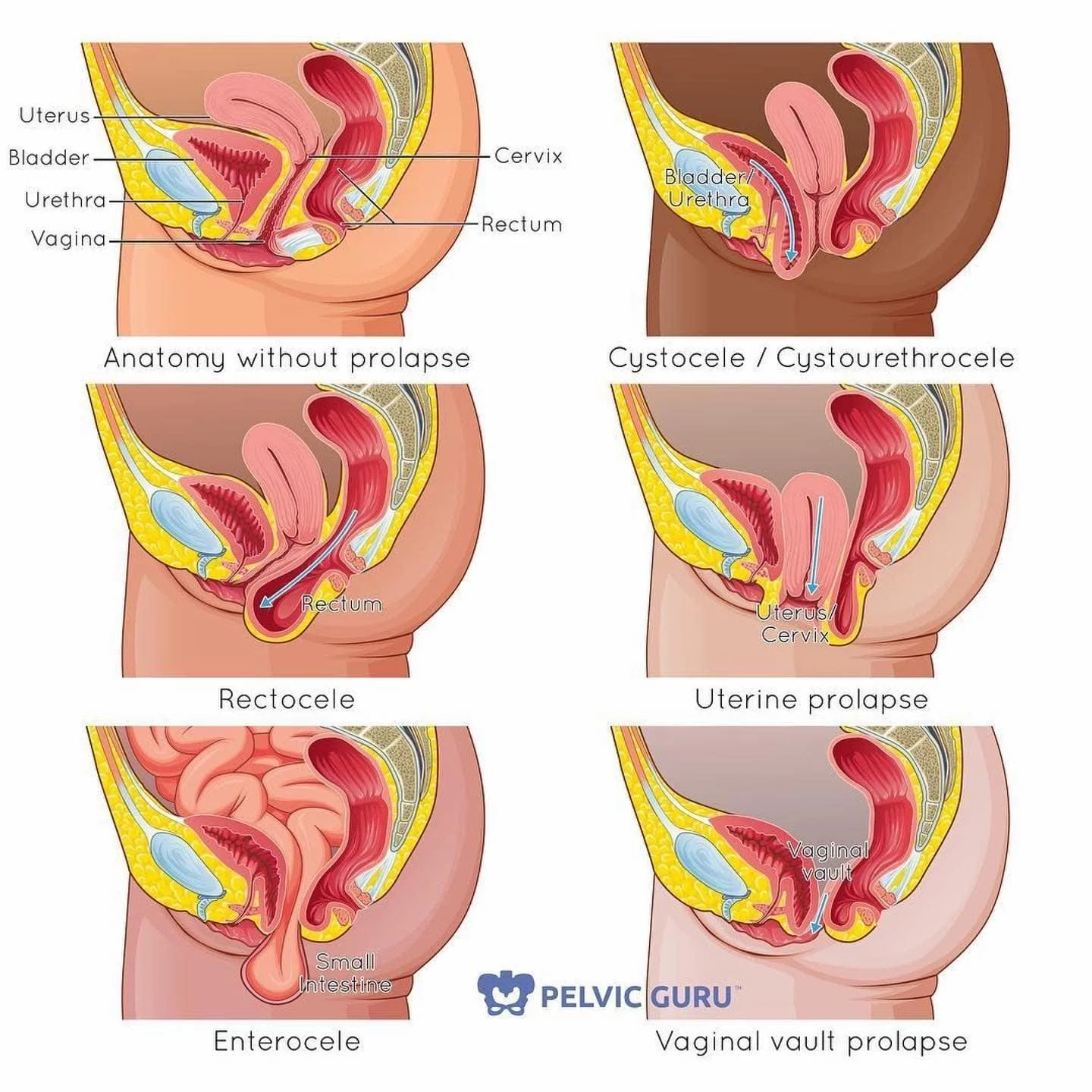
Cystocele: This one's like your bladder saying, "I need a break!" It sags into the front vaginal wall.
Rectocele: The rectum takes a detour into the back vaginal wall. It's like your rectum decided to be a bit adventurous.
Uterine Prolapse: Ah, the uterus – the queen of the show. It decides to go on a downward journey into the vaginal canal.
Enterocele: This is the small intestine, thinking it's on a vacation and poking into the vaginal space.
Vaginal Vault Prolapse: After a hysterectomy, sometimes the top of the vagina can drop down. It's like the empty palace after the queen is gone!
Symptomatic Prolapse: The How It Feels
Now, let's switch gears to symptomatic prolapse. This one's all about the "how it feels." Symptomatic prolapse focuses on the symptoms and discomfort that these organ migrations can cause.
Here's the deal:
Feeling the Pressure: When your organs decide to shift, they might push on your vaginal walls or even make their way outside the body. It's like having a tiny (or not so tiny) friend camping out where they shouldn't be.
Urinary Troubles: If your bladder is involved, you might experience frequent urination or leakage. Say hello to those unexpected bathroom visits.
Bowel Blues: When the rectum is in the picture, it can lead to constipation, incomplete emptying, or even fecal incontinence. Not the kind of "going with the flow" we want!
Pelvic Pain: Aches and discomfort in your pelvic region can be a part of the symptomatic prolapse package.
Backache: Lower back pain might join the party if your uterus or other organs are taking a road trip.
Grade Matters: The Prolapse Hierarchy
Now, let's introduce the concept of grading. It's like rating movies, but for prolapse. Grades help to determine the severity of prolapse, and it's your pelvic floor therapist's job to assess it. Here's a simplified version:
Grade I: This is the mild stage where your organs have just started their adventure.
Grade II: A bit more noticeable, with organs reaching further into the vaginal canal.
Grade III: Things are getting serious now, with organs almost making their way out of your body.
Grade IV: The grand finale – this is the most severe stage where organs are completely outside the body. Not the kind of show we want to attend!
Treatment and Management
Now, for the good news – prolapse can be managed and treated! Whether it's pelvic floor exercises, a pessary, lifestyle adjustments, or even surgical options, there's hope. Your pelvic floor therapist will be your trusty guide on this journey.
So, in the grand scheme of things, understanding the differences between anatomical and symptomatic prolapse is crucial for navigating your pelvic health journey. It's like being the captain of your own ship, steering it away from the rough waters of discomfort and complications.
Remember, you're not alone in this – there's a whole community of moms and professionals cheering you on. And if you ever feel like your pelvic organs are misbehaving, don't hesitate to reach out to your friendly neighborhood pelvic floor therapist. They'll help you get back on the path to pelvic health glory!
So here's to you, amazing moms, steering the ship of your pelvic health journey with humor, determination, and a dash of education. Happy healing! 🌟